Your Guide: How to Create a High-Performing Infusion Solution
Fragmented infusion services result in lost revenue and poor patient care. Creating a site of care strategy, that includes infusion suites and home infusion options, helps health systems regain control in order to reduce patient leakage and improve overall outcomes. This guide shares the essential steps to launch—or optimize—a patient-centered infusion model that delivers measurable value.
The Real-World Detriment of Infusion Gaps
Imagine this: a patient in your health system requires a specialty infusion for a complex condition like multiple sclerosis. Referrals bounce between departments, prior authorizations stall, and the patient isn’t sure where or when they’ll receive treatment. Despite this being a critical treatment, the process leaves the patient confused, misinformed, or delayed in getting care. Meanwhile, the health system isn’t able to properly manage the patient’s condition and loses out on revenue.
“Millions can be lost annually due to missed infusion opportunities,” explains Erick Siegenthaler, Visante’s Senior Director. “This is where health systems can reclaim revenue.”
In addition to additional revenue, establishing the right process and sites of care enables health systems to reclaim value in the form of better patient outcomes by solving the leakage challenge.
The Benefits of an Integrated Infusion Model: High-Touch Care, High-Impact Results
An intentionally designed infusion service line is a strategic asset that drives positive results, including:
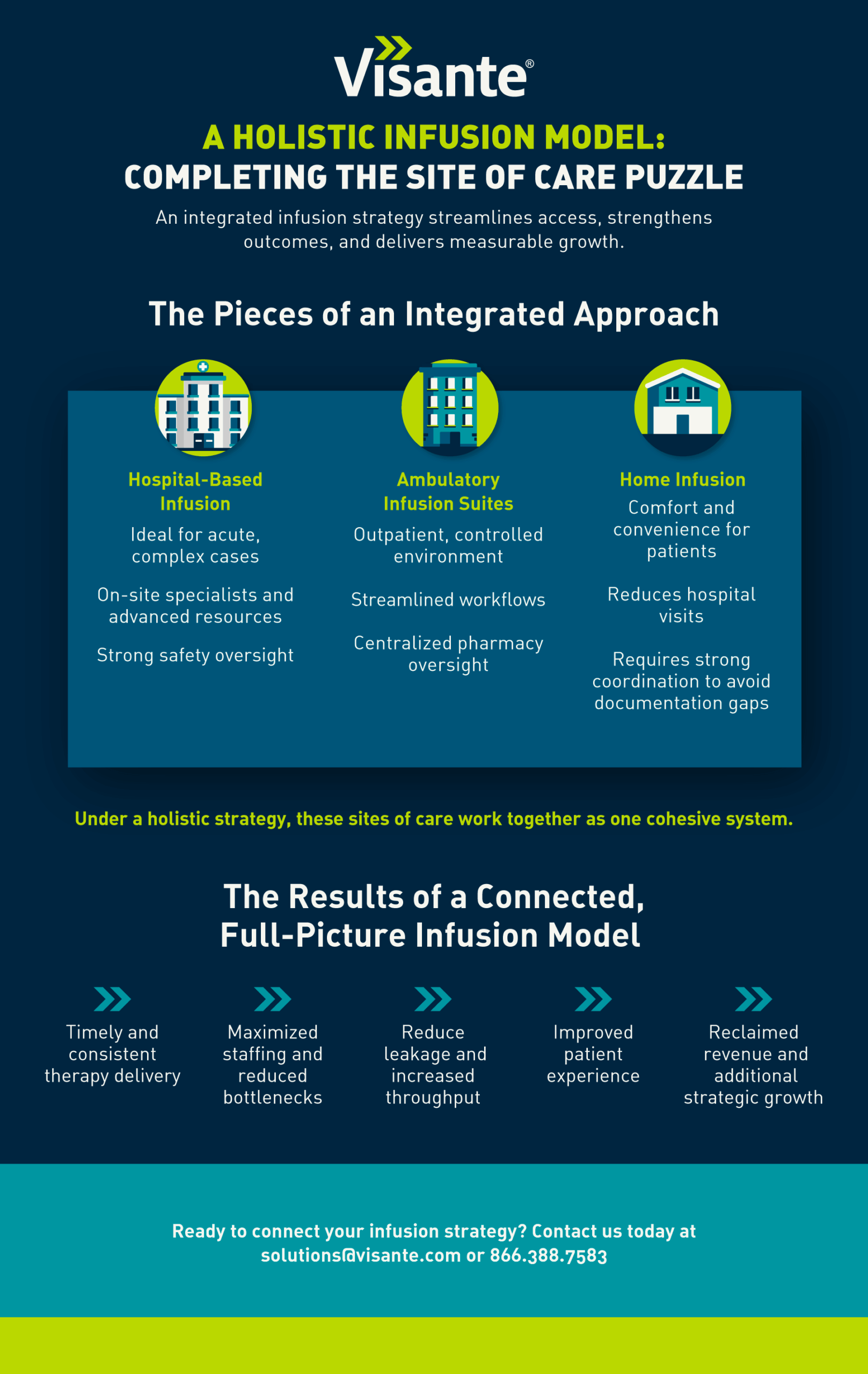
- Holistic Patient Care Across All Sites of Service: An integrated infusion strategy empowers your organization to deliver seamless, patient-centered care, whether in a hospital-based setting, an ambulatory infusion suite (AIS), or the patient’s home. Managing the entire journey from diagnosis to treatment and medication fulfillment supports better coordination.
- Improved Clinical Outcomes Through Centralized Oversight: With an integrated infusion model, health systems can streamline medication access and administration across all care sites. This leads to reduced delays, minimized errors, and consistent care delivery.
- Operational Efficiency Across Channels: Leveraging each infusion site strategically optimizes resource allocation, reduces bottlenecks, and enhances scalability.
- Reclaimed Revenue and Strategic Growth: Managing high-cost, high-impact therapies across multiple infusion settings enables health systems to reduce service leakage, increase throughput, and unlock new revenue opportunities.
Building the Foundation of a Thriving Infusion Solution
When implementing an infusion strategy, it’s essential to integrate both operational and clinical care elements. For example, to lay the groundwork for a successful infusion strategy, you must have:
- Support for High-Impact Therapies: Infusion suites are designed to deliver complex, high-touch treatments—often specialty medications—safely and efficiently.
- Coordinated Care Across the System: A dedicated, cohesive team can effectively manage medication access, prior authorizations, and coordination across departments. Integrating systems like Epic and MyChart is key for continuity of care and improving patient communication.
- Accreditation: To meet payer requirements and deliver high-quality care, pursuing accreditation from recognized bodies like ACHC, URAC or The Joint Commission is highly recommended.
- Efficient Staffing & Operations: A combination of nurses, pharmacists, and care coordinators is essential to running a successful infusion service line.
“Infusion care is one of the most complex areas in pharmacy, requiring deep expertise across various domains,” Siegenthaler states.
Key Considerations Before Getting Started with Your Comprehensive Infusion Solution
Developing a comprehensive infusion strategy is a complex undertaking that requires planning across multiple domains. Here are four critical areas to evaluate before moving forward:
Which Infusion Model Should I Choose?
Designing an effective infusion program starts with selecting the right combination of care settings based on your patient population, geographic reach, and operational capabilities. While many health systems already have established hospital-based infusion sites, it’s important to weigh the benefits of ambulatory infusion suites and home infusion services, too.
Ambulatory infusion suites, often led by pharmacy teams, offer a controlled outpatient environment that supports centralized oversight, optimized workflows, and seamless Electronic Health Record (EHR) integration.
Home infusion, on the other hand, provides convenience and comfort for patients. However, without the right strategy in place, it can introduce some documentation complexity and coordination challenges. That’s why it’s critical for health systems to adopt a holistic infusion strategy that integrates both home and ambulatory settings.
Health systems increasingly benefit from implementing a hybrid model that spans multiple sites of care. For example, a health system with multiple outpatient and specialty sites can improve access, patient experience, and revenue by combining home infusion, AIS, and hospital-based care into one coordinated strategy.
Who Do I Need to Staff My Infusion Service Line?
You’ll need specialized nurses, pharmacists, and support staff who are well-versed in sterile compounding and patient care. Consider whether to use in-house staff or rely on contract nursing.
What Do I Need in Place for Revenue Cycle Management?
Comprehensive infusion solutions involve both medical and pharmacy benefits, making revenue cycle complexity a common challenge. To optimize healthcare revenue cycle performance, it’s essential to streamline billing workflows and integrate them across departments and systems. A coordinated approach results in accurate reimbursement, minimized delays, and long-term financial sustainability.
How Can 340B Strengthen My Infusion Strategy?
The 340B program plays a critical role in improving access to high-quality infusion care. By reducing drug acquisition costs, it empowers covered entities to reinvest in patient services—expanding reach, enhancing outcomes, and supporting a more patient-centered care model.
Measuring Success: How to Track the Value of Your Infusion Services
Evaluating the performance of your infusion services is essential to achieving long-term success. Track these KPIs to measure your impact:
- Turnaround Time: How quickly can infusions be administered to patients?
- Patient Satisfaction: Are patients satisfied with the care they receive?
- Revenue Generation: Track the revenue generated through infusion therapies, especially high-cost treatments.
- Operational Efficiency: Are staffing and resources utilized effectively?
- Clinical Outcomes: Are patients receiving timely, appropriate therapy that leads to improved outcomes?
If you’re unsure how to track these KPIs—or if your current metrics aren’t giving you the full picture—Visante can help. Our experts work alongside your team to optimize data integration and uncover actionable insights that drive continuous improvement. Reach out to learn how we can support your clinic’s ongoing success.
Visante’s Role in Your Infusion Journey
“Building an infusion strategy is complex, but Visante can help guide you through every step of the process,” Siegenthaler explains.
Our experts specialize in customizing infusion solutions that fit your health system’s needs. Whether you’re just starting or optimizing your current model, we can streamline your path to success.
Ready to Take the Next Step?
At Visante, we’ve seen firsthand the powerful impact an integrated approach can have on a health system. Whether you’re launching new pharmacy-based services or optimizing an existing hospital infusion center, our experts will guide you in achieving operational and financial success. Contact Visante to learn how we can help you build a high-performing, patient-centered infusion strategy.
