The Reality of Drug Diversion in Health Systems
Drug diversion is a stark and sobering reality in healthcare. Even the most trusted, patient-centered team members can be at risk. If substance use disorder (SUD) exists in the community, it almost certainly exists within the hospital. And for those working on the front lines—where proximity to controlled substances is constant—the vulnerability is amplified.
Lingering Risks from Pandemic Protocols
COVID-19 reshaped healthcare in countless ways, but it also left behind new vulnerabilities. During the pandemic, relaxed DEA and hospital protocols—such as loosened telemedicine rules, expedited DEA registrations, and accelerated staff onboarding—were necessary to maintain patient care. Yet these well-intentioned measures also reduced safeguards. Many remain in place today, prolonging exposure to diversion risks.
The Diversion Triad: A Framework for Understanding Risk
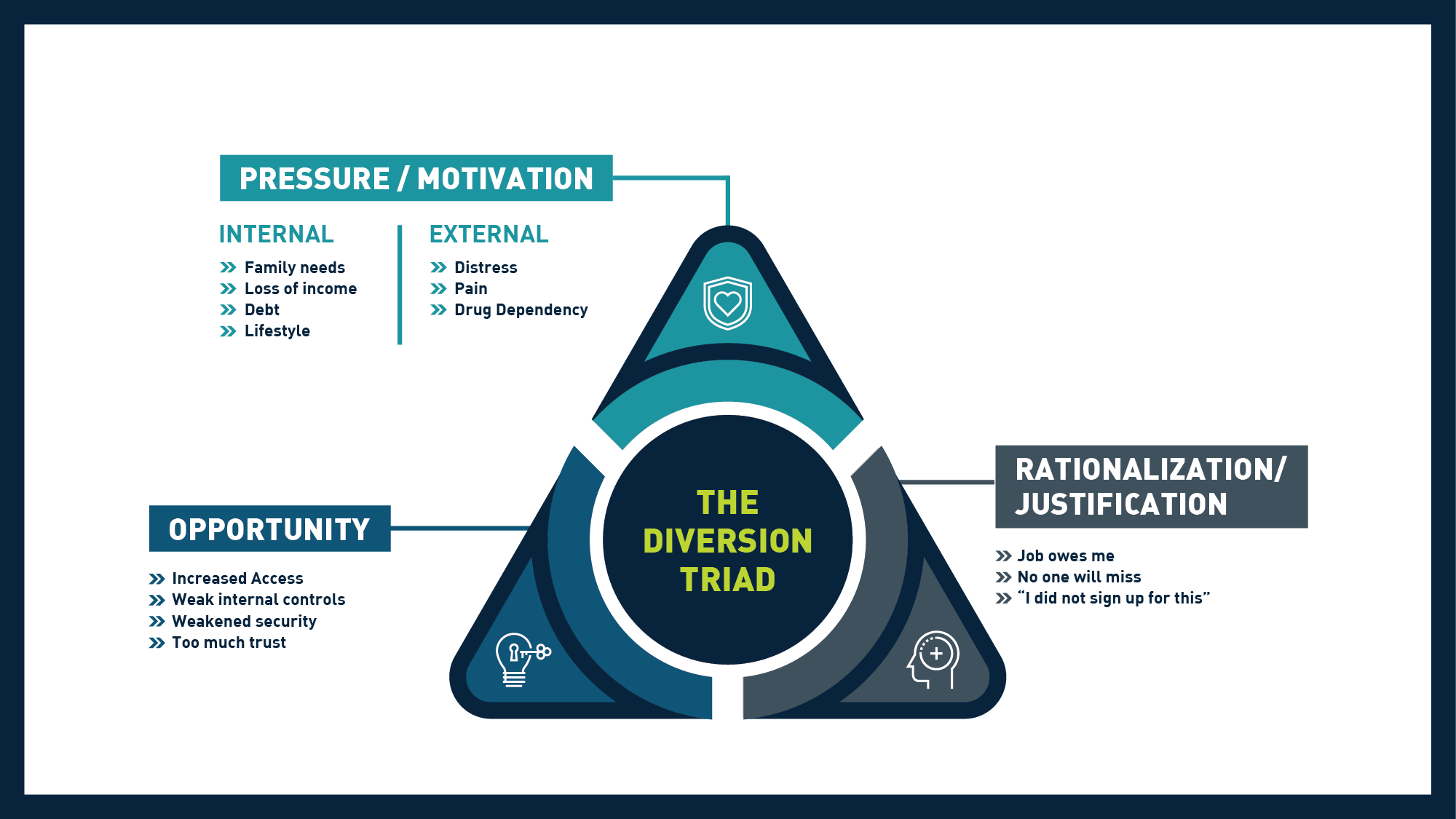
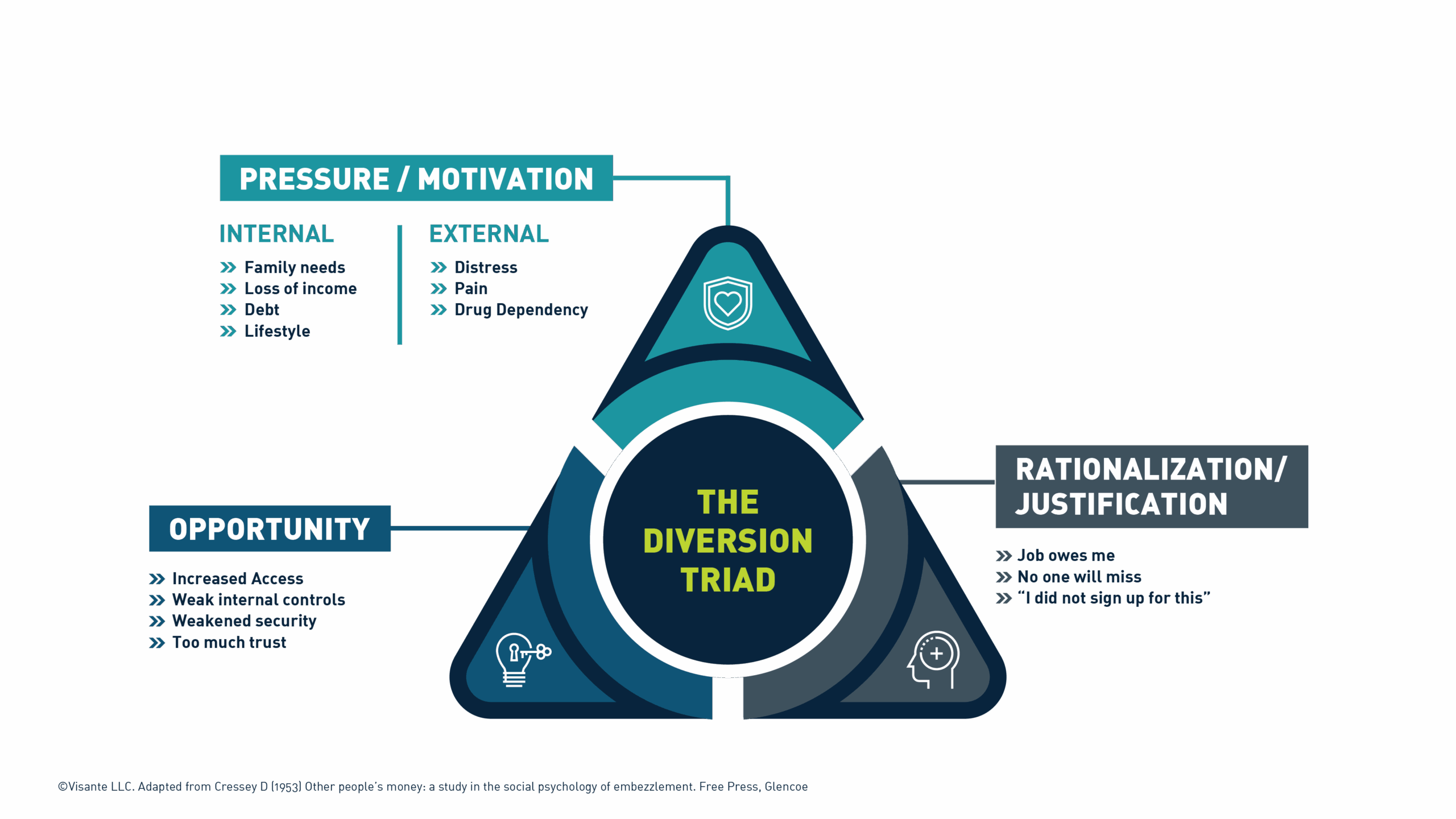
To fully understand diversion, it’s important to move beyond the notion of “bad actors.” Visante’s Diversion Triad, adapted from Donald Cressey’s Fraud Triangle (1953), reframes diversion as a type of fraud, just with a different currency.
Drug diversion typically emerges when three factors align:
- Opportunity: Gaps in oversight or workflows create access points.
- Rationalization: Personal justifications make the behavior “acceptable” to the individual.
- Pressure: Internal or external stressors fuel the decision to act.
This framework underscores that diversion is rarely about malice. More often, it reflects how vulnerable individuals, working in high-pressure environments, can succumb when conditions converge.
The Leadership Imperative
Preventing diversion isn’t just a matter of compliance. It’s a matter of culture, vigilance, and leadership. Health system leaders must acknowledge that:
- The risk of diversion is closer to home than many expect.
- Strong, comprehensive diversion prevention programs are an investment in safety, trust, and organizational integrity.
- Closing blind spots in oversight and workflows is critical to reducing risk.
When leaders prioritize proactive prevention, they protect patients and staff while reinforcing public trust in their institution.
A Path Forward
Building a robust diversion prevention program is complex, but the payoff is invaluable: safer patients, supported staff, and preserved financial stability. At Visante, our experts partner with health systems to design and implement sustainable prevention strategies. From risk assessments and policy development to advanced monitoring and ongoing oversight, we help organizations stay ahead of risk.
The reality is clear: drug diversion can happen anywhere. The question is whether your health system is prepared. Let’s safeguard your organization together—reach out to Visante today.
